Sleep and Inflammation: Why Poor Sleep Fuels Chronic Illness
- CSMA Team

- Aug 24, 2025
- 3 min read
Updated: Sep 3, 2025
Chronic illness is on the rise in America. According to the CDC, 6 in 10 adults live with at least one chronic disease, and 4 in 10 live with two or more. At the core of many of these conditions—whether heart disease, diabetes, arthritis, or autoimmune disorders—is a common culprit: inflammation.

While inflammation is the body’s natural defense against injury and infection, when it becomes chronic, it fuels disease instead of healing.
One surprising but critical factor that drives inflammation? Poor sleep.
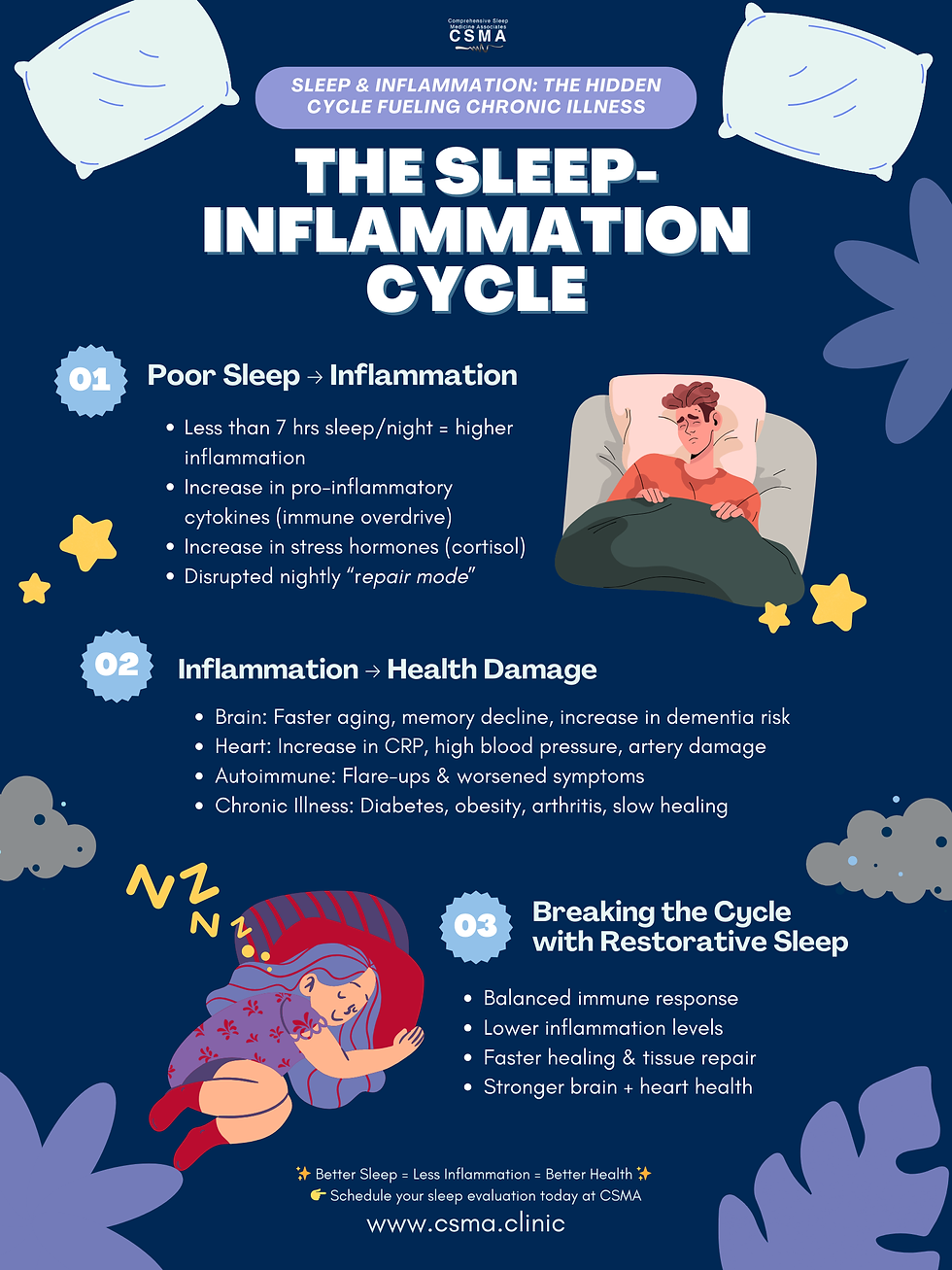
The Link Between Sleep and Inflammation
Sleep isn’t just a time for rest—it’s when your body goes into repair mode. During deep sleep, the immune system regulates cytokine production, the proteins that help control inflammation. But when sleep is disrupted or insufficient:
The body produces higher levels of pro-inflammatory cytokines, tipping the immune system into overdrive.
Stress hormones such as cortisol stay elevated, compounding inflammatory responses.
The natural balance between recovery and immune defense is thrown off, leaving the body vulnerable.
In fact, studies show that people who consistently get less than 7 hours of sleep per night are at greater risk of developing obesity, diabetes, cardiovascular disease, and even autoimmune disorders—all of which are tied to inflammation.
Chronic Illness and Inflammation in America
The numbers tell a sobering story:
Heart disease and stroke, both inflammation-driven conditions, remain the leading causes of death in the U.S.
Autoimmune disorders affect nearly 50 million Americans, with research showing that disrupted sleep can trigger flare-ups and worsen symptoms.
Type 2 diabetes, strongly linked to both obesity and poor sleep, is increasingly prevalent and carries inflammation at its core.
When poor sleep is part of the picture, these illnesses often intensify, slowing healing and lowering quality of life.
Sleep, Inflammation, and Your Brain
Your brain is one of the first places poor sleep and inflammation leave their mark. Research shows that chronic inflammation accelerates brain aging, damaging neurons and reducing the brain’s ability to repair itself. Over time, this can lead to memory lapses, slower processing speed, and difficulty focusing.
Poor sleep also interferes with the brain’s “glymphatic system”—the nightly cleaning process that clears out toxins and inflammatory waste products. When that system is disrupted, harmful proteins such as beta-amyloid accumulate, raising the risk of Alzheimer’s disease and other forms of dementia.
Simply put: lack of sleep and excess inflammation don’t just make you feel foggy—they can actually age your brain ahead of its time.
The Hidden Heart Risks
Your heart and blood vessels are also highly sensitive to both sleep and inflammation. People who consistently sleep less than 7 hours per night show higher levels of C-reactive protein (CRP), a key marker of inflammation strongly linked to heart attack and stroke. Sleep deprivation also raises blood pressure, stiffens arteries, and disrupts heart rate variability—all signs of cardiovascular stress.
Combined, these factors create the perfect storm: inflammation damages the lining of blood vessels while poor sleep prevents the body from repairing them. This helps explain why people with untreated sleep disorders, such as sleep apnea, face significantly higher risks of hypertension, arrhythmias, and heart disease.
How Better Sleep Reduces Inflammation
The good news is that improving sleep health can directly reduce inflammation. Patients who address sleep disorders such as sleep apnea, insomnia, or restless leg syndrome often see measurable improvements in inflammatory markers.
Benefits of restorative sleep include:
Lower levels of inflammatory cytokines
Improved blood sugar regulation
Reduced risk of flare-ups in autoimmune conditions
Faster healing and tissue repair
Simple steps to create optimal sleep hygiene, like maintaining a consistent sleep schedule, reducing screen time before bed, and creating a restful environment, can help. But for those struggling with ongoing sleep issues, professional evaluation and treatment are essential.
Take the First Step Toward Healing Inflammation and Sleep Health
If poor sleep is fueling your health problems, it may be time to dig deeper. At Comprehensive Sleep Medicine Associates (CSMA), we specialize in identifying and treating sleep disorders that contribute to chronic inflammation and illness. Our team of sleep medicine experts—led by Dr. Jerald H. Simmons, a pioneer in the field—will guide you toward healthier, restorative sleep.
Contact CSMA today to schedule your sleep evaluation and take the first step in reducing inflammation, reclaiming your health, and restoring balance to your body.





Comments